Harmony Multani
New research at John Hopkins University found COVID-19 can destroy brain cells if it is able to get past the organ’s natural defensive blood brain barrier.
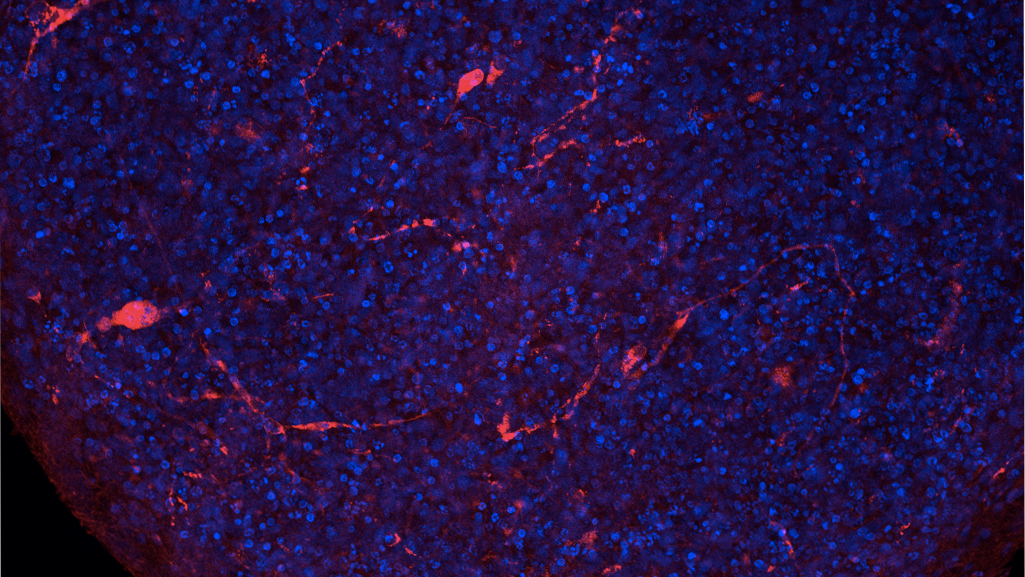
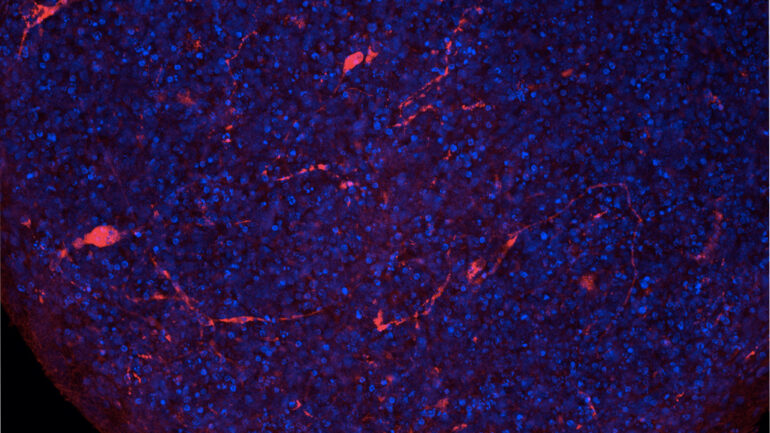
The research, which used organic mini brains models made from stem cells and no bigger than the tip of a ballpoint pen, showed if COVID-19 can get past the barrier it can quickly replicate in brain cells, killing them off.
“The brain is apparently killing these infected cells and throwing the infection into other cells which can be then be infected again,” Dr. Thomas Hartung, professor of toxicology at John Hopkins University, who worked on this research.
The barrier regulates the movement of cells between the blood and the brain, allowing for the organ’s proper function and protects nervous system tissue from toxins, viruses and bacteria.
Hartung said the research uncovered a new need to focus on embryo development in pregnant women who have been infected with COVID-19. Similar to the mini brains, embryos less than 12 weeks old have not yet developed their own barrier, he said.
“So an embryo would be at risk, and others have already shown that the virus passed the placenta,” Hartung said. But the issue is “babies who were exposed to the virus in the first 12 weeks of embryo development, have not yet been born.”
He said there is no immediate way to compare the findings of the mini brains to human development, because certain diagnoses like the potential of autism in newborns whose mothers were infected by the virus may take some time to set in.
“This is only the first step in saying, ‘okay guys, all of us in the scientific community should now start looking into what are the consequences of this,’” Hartung said.
He said the brain is special in the sense that brain cells do not regenerate, so “whatever this specific cell was apart of, let’s say a certain memory or a certain response pattern, we learned that this can be wiped out.”
The report stated this research used the same model of a mini BrainSphere as researchers applied while studying the Zika virus, Dengue HIV and John Cunningham virus infections.
John Hopkins’ researchers incubated the mini-brains with COVID-19 for six hours, and within 72 hours the virus began replicating quickly.
“Immune cells which typically gets rid of infected cells don’t enter the brain, so we call this immuno privilege, which means that the brain is spared from these inflammatory responses,” he said.
“The problem is, this can allow viruses to stay in the brain,” Hartung said.
The study’s researchers noticed “at least a tenfold increase in the virus copies per total RNA” which allowed researchers to demonstrate the “potential critically important neurotropism of SARS-CoV-2.”
Hartung said Johns Hopkins is now working on research that focuses on whether it is possible to rid the brain of COVID-19 once infected.
Comparing it to HIV, Hartung says that doctors can get rid of HIV with treatment in every part of the patient’s body, except the brain — as soon as the patient stops taking the medication there is a possibility the virus or infection will begin repopulating.
The research presented unique issues as Hartung said “the human brain is almost impossible to obtain as a living thing.
“We were the first group to mass produce them, because this was really opening up for testing of drugs, testing of of toxic effects of substances, they also have been looking into other diseases from Alzheimer’s to Parkinson’s to Cancer, but we also did some work on virus infections,” he said.