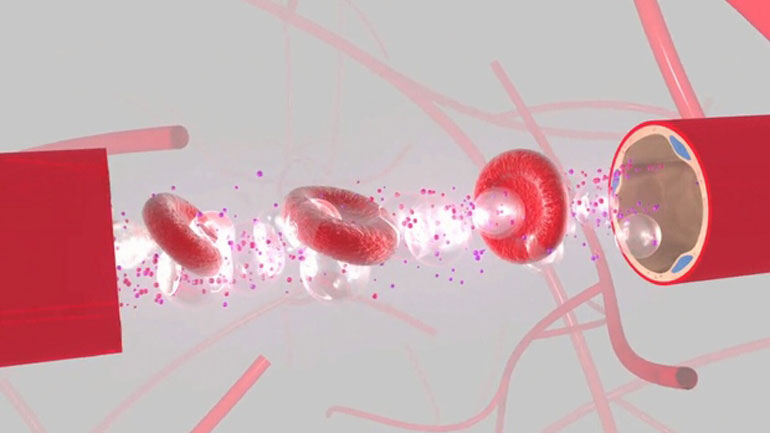
Focused ultrasound technology creates micro-bubbles in patients’ bloodstreams. This allows doctors to safely administer life-saving drugs that will treat brain-disease. Photo courtesy of Columbia Engineering.
By Nicole Williams
Scientists at Sunnybrook Health Sciences Centre are the first to use a new procedure that will deliver life-saving drugs to the brain without invasive surgery.
The new method uses focused ultrasound technology to non-invasively breach the blood-brain barrier, a sheath that protects blood vessels in the brain.
Allison Bethune is a clinical research co-ordinator at Sunnybrook’s neurology department, and was a part of the team who researched this new treatment.
“It has the potential for scientists to more effectively treat brain tumours, Parkinson’s and Alzheimer’s and other brain diseases without the risks associated with invasive surgery,” Bethune told Humber News.
“This technique will open up new opportunities to deliver potentially much more effective treatments to the targeted areas,” said Todd Mainprize, the principal investigator in the study, in a statement.
Bethune explained that the process begins with an MRI machine that opens the blood-brain barrier where micro bubbles are injected into the blood stream and timed with an ultrasound beam that targets blood vessels in the brain. When the bubbles arrive and hit the beam, they become excited and loosen the cells, opening the barrier temporarily to allow medications to reach their targeted location.
“Breaching this barrier opens up a new frontier in treating brain disorders,” said Dr. Neal Kassell, chairman of the Focused Ultrasound Foundation.
The first patient to undergo this new technique was Bonny Hall who has had a benign brain tumour for eight years that became malignant. She is the first of 10 patients with brain tumours who have been listed for the treatment.
Hall’s tumour is classified as a glioma, which spreads out into a web-like shape that is difficult to remove in surgery. Often parts of the tumour are left behind, which is the reason survival rates for gliomas are particularly low.
With this new technique, chemotherapy drugs will have access to the cancer that remains.
Hall underwent surgery at Sunnybrook earlier this week and Mainprize said the new technique worked “exactly as hoped.”
Bethune said the treatment is still very much in the research phase and it could remain that way for up to two more years.
“We need to determine its safety and feasibility first,” said Bethune. “But we already have a large number of patients phoning in to see if they can get the treatment.”